A common presentation in orthopaedics is hip osteoarthritis. Here we will answer frequently asked questions about this condition.
What is hip osteoarthritis?
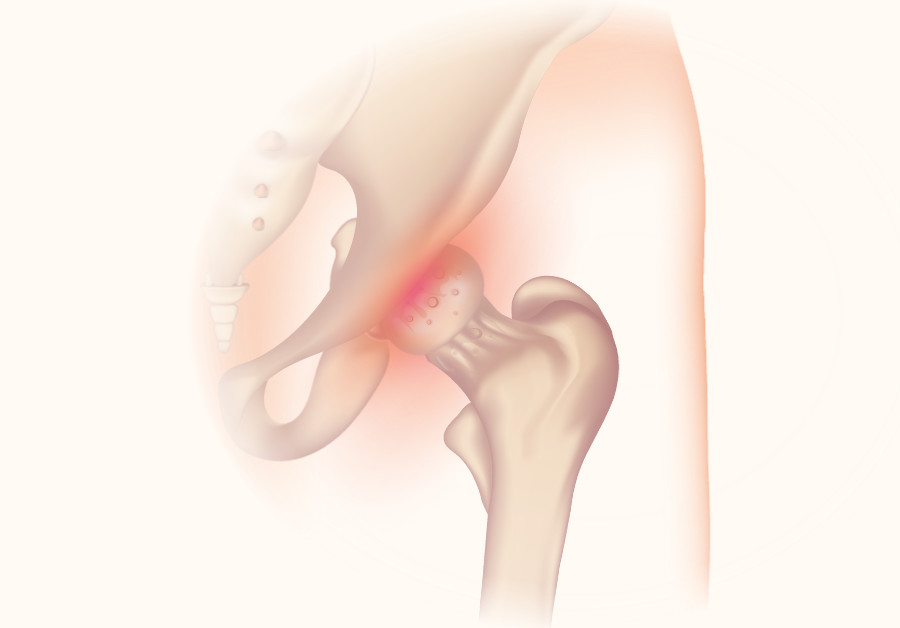
Osteoarthritis can develop in any joint in your body. The hip joint is where the top of your thigh bone connects with your pelvis. In between the bones there is cartilage, which is softer and allows the bones to move against each other smoothly. Osteoarthritis is where this cartilage wears away over time (“degeneration”), creating friction between the bones. This can feel like stiffness or pain in your hip. It can lead to small nubs of bone growing in the joint (known as a bony spur or “osteophyte”) which can also cause pain when they rub together. The cartilage breaking down means the bones in the joint move closer together leading to reduced range of movement in your joint.
As well as pain and stiffness, your hip may feel unstable, swollen or tender. You may struggle to walk or sit, or you may hear noises when you move the joint as the articulating bones rub together. The pain often tends to get worse the more you use the joint. This type of pain normally develops gradually over months.
What factors make you more at risk of hip osteoarthritis?
Osteoarthritis is more common in those over 50 years of age, more common in women, and more common in those who are overweight. You may have a family history meaning that relatives also might have had osteoarthritis. Some careers involving sports or manual labour could lead to overuse or early wear and tear of the joint, or it is common if you have previously had an injury (trauma) to that joint. If you had rheumatoid arthritis or gout in a joint you may be more likely to get secondary osteoarthritis.
How is hip osteoarthritis diagnosed?
The symptoms of arthritis will be part of a “clinical history” taken by your doctor which paints a picture of what might be affecting your hip joint, and a physical examination where the doctor will check your range of movement and power. An x-ray or an MRI might be taken to look at the bones within the joint. Blood tests or tests on the fluid in the joint may confirm that it is not a different type of arthritis.
How is hip osteoarthritis treated?
If your hip pain is made worse by exercise or activity, you should rest and return to exercise gradually. Gentle, low-impact exercise may strengthen the muscles around the joint, including yoga or swimming which may be beneficial for hip pain. You can take over the counter painkillers according to the dosage guidelines; ibuprofen should always be taken with food. Over the counter pain-killing creams such as ibuprofen gel or Deep Heat may also soothe the joint. Apply ice packs or heat for 20 minutes at a time.
Physiotherapy or chiropractic adjustment may help as they can give you exercises to stretch or strengthen the muscles around the joint. Occupational therapists can help you find ways to do daily activities with adjustments, such as special chairs or hand rails to help use the stairs. If you struggle to walk, walking aids or orthotics (insoles in your shoes) may help.
How do you know when to see a specialist about hip osteoarthritis?
As the symptoms develop gradually, you may not know when the best time to ask for medical advice is. If you are worried about hip pain or stiffness, or if the symptoms are limiting your daily activities, you should consult a healthcare professional such as your GP, or a physiotherapist. You may be referred to a specialist doctor such as an orthopaedic surgeon for diagnosis and treatment options. If your pain limits your ability to work, you should contact occupational health who will discuss with you what adaptations can be made until your knee has recovered.
Conclusion
Hip osteoarthritis is a common but challenging medical condition and if your symptoms have not settled, get in touch or call 0161 772 961 to book in now for an assessment and to discuss treatment options with Mr Kumar.



